One of the biggest ‘complications’ of hernia surgery is that the hernia can return after it has been repaired, and is called a ‘recurrent’ hernia. This happens to EVERY surgeon; no center has 100% success, including ours. However, there is clear evidence based on medical studies that certain factors can impact a patients chance of developing a recurrent hernia.
At California Hernia Specialists we offer all possible options for definitive repair. This includes basic open repair, laparoscopic repair, and more advanced component separation and advanced mesh repairs. Our center falls into the lowest risk category for developing a recurrent hernia as you will read about below.
Hernia Types – Recurrent – Causes
Although patients often cannot affect their risk of developing a primary (first time) hernia, they actually can impact their development of a recurrent hernia. Recurrent hernias are ones that form after a surgeon has already attempted to repair the primary hernia. This can happen as early as days/weeks after the first surgery, or as long as decades. Regardless, there are important steps a patient can take to minimize their chances of having a recurrent hernia. The risk factors for developing a recurrent hernia after a primary repair include
- Low surgical volume of hernia repairs by the surgeon performing the initial operation
- Surgical inexperience of the initial surgeon
- Open hernia surgery under local anesthesia
- Insufficient surgical technique of the surgeon including:
- lack of mesh overlap
- improper mesh choice
- lack of proper mesh fixation
- Presence of a sliding hernia
- Collagen disorders
- Obesity
- Chronic steroid use
- Activity too early after surgery
- Smoking, COPD, chronic cough
- No mesh is used for initial repair
- Initial mesh not fixed to muscle strong enough
The HerniaSurge group’s International Guidelines point to at least 4-5 different risk factors for hernia recurrence which are influenced by a patients surgeon. The best way a patient can help prevent a hernia recurrence is to find a surgeon who performs a high volume of hernia surgeries. This volume of surgeries clearly imparts a high level of surgical experience which can reduce a patients chance at developing a recurrent hernia.
Patients can read more about recurrent hernias and their causes from the International Guidelines for Inguinal Hernias:
Laparoscopic Recurrent Hernia Repair
Recurrent hernias can be good candidates for laparoscopic hernia repair. This is because the muscles around the hernia are obviously weak; so much so that the muscles tore after an attempted repair. By using laparoscopic techniques, a larger piece of mesh can usually be placed allowing for all the weakened muscleto be repaired. Also, if the original surgery was done open, by operating laparoscopically previous scar tissue can be avoided.
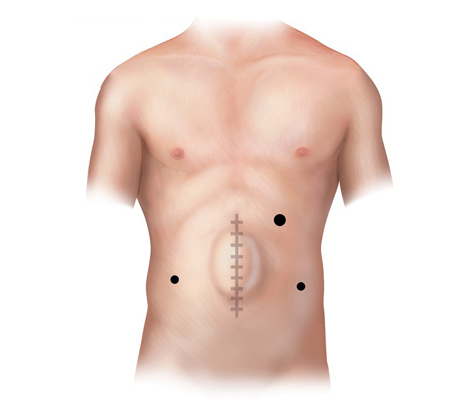
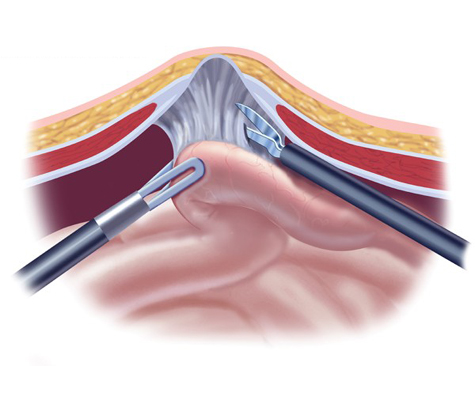
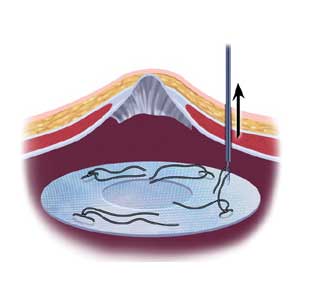
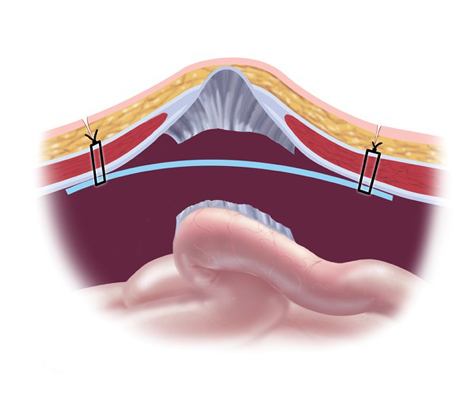
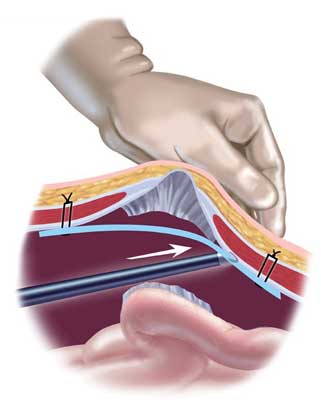
A hernia mesh is rolled and placed through one of the laparoscopic ports into the abdomen. From there, it is pulled up against the muscle surrounding the hernia with stitches (sutures). Once the mesh is secured in place with about 4 sutures, a special stapling device is used to further fix the mesh to the healthy muscle.
Common Concerns Regarding Recurrent Hernias
Sometimes a patients hernia is so large that a laparoscopic repair will not provide a suitable repair of the FUNCTION of the abdominal wall. With some laparoscopic repairs, the muscles are left open and are not closed. This works very well in patients with small sized hernias. But once the hole becomes larger, placing apiece of mesh across a very large hole will not return the abdominal wall to a suitable functional state; there will always be a large bulge.
This is obviously not desirable. In these advanced cases, an open approach is required. By doing surgery open, the muscles can often be pulled back together. This sometimes requires advanced techniques (component separation) to allow a tension free repair. A mesh can be placed under the muscle and sometimes over the muscle to reinforce the repair for years to come and help prevent another recurrence.
Statistics have shown that every time a hernia is repaired, and then recurs, the chances of recurrence again after another surgery increases dramatically. For patients who have already had 3-4 hernia repairs, the chances the hernia can come back after another surgery can be almost 50%! This is clearly why having the hernia fixed the correct way, the first time, is so desirable.
Complications after recurrent hernia surgeries are also much more common. Whether it’s a relatively small inguinal hernia or umbilical hernia recurrence, all the way up to large ventral hernias, there are increased risks. Obviously there becomes an increasing amount of prior scar tissue which makes the surgery more difficult. Often there are already old pieces of mesh which have been placed in a previous effort to reduce the chance of a recurrent hernia. All of these cause the surgery to be more difficult, which in turn increases the chances of complications.
Recurrent Hernia Case Reports:
At California Hernia Specialists, we have seen a high number of complicated cases over our many years in practice. This gives us a depth of knowledge and experience often not seen in other surgery practices and with other surgeons.
Below are a list of complex cases specific to recurrent hernias. Patients can also read more about unique cases that we have treated on our ‘Recent Case Highlights‘ page.
1. Laparoscopic repair of recurrent incisional hernia in a 74 year old doctor.
A 74 year old physician had a large pelvic tumor removed which was non cancerous. She developed a hernia 2 years after her surgery and underwent a laparoscopic incisional hernia repair at a large University Hospital in Southern California. Weeks after her surgery, she noticed a recurrent bulge in the lower part of her abdomen.
She presented to California Hernia Specialists for evaluation and treatment. On examination she had a 1-2 inch bulge in the lower abdomen, just above her pubic bone. This recurrent incisional hernia was painful when she exercised and while she was at work. We offered her laparoscopic recurrent incisional hernia repair.
Laparoscopic Ventral Hernia Repair
Dr. Harris narrates a laparoscopic incisional hernia repair.2. Open recurrent umbilical hernia which failed 2 prior surgeries.
This patient had been operated on two previous times by an outside surgeon. The first surgery was done without mesh. After it recurred almost immediately, the same surgeon used a ‘large piece of mesh’ as was described by the patient and the operative report. Unfortunately shortly after this surgery, the bulge returned and the patient developed increasing pain.
The patient presented to California Hernia Specialists for a second opinion before returning for a third surgery. The patient underwent a physical exam and a CT scan to evaluate the size of the hernia. A number of options were presented to the patient and ultimately it was decided to treat him with an open recurrent umbilical hernia repair.
A ‘tummy tuck’ incision was used to help tighten and remove excess skin and the old scar.The old mesh had completely separated from the muscle and was stuck to the small intestines internally. Careful removal of the mesh was required to free the intestine from the hernia.The muscle was closed and a new piece of advanced mesh was placed under the muscle to reinforce the repair. The images below are from before and after his hernia surgery.
This image shows photos before his surgery along with the CT image corresponding to his hernia. The arrows point out the obvious hernia.
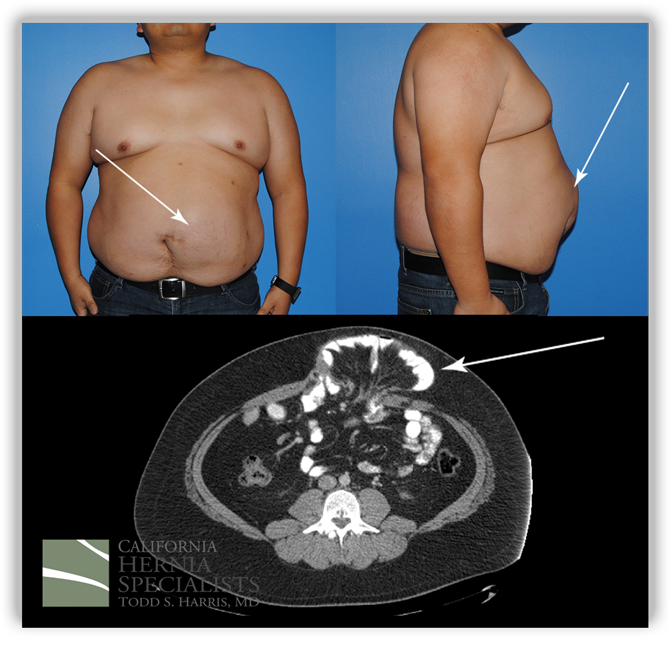
Click here for more images and pictures
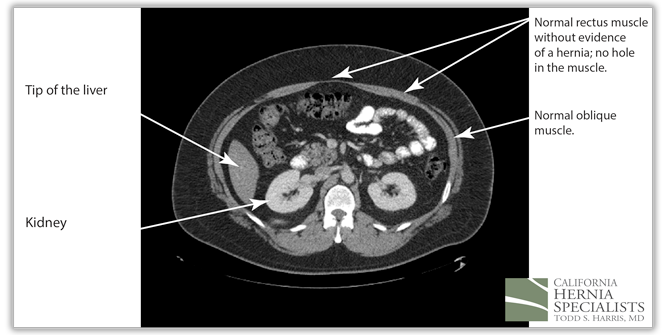
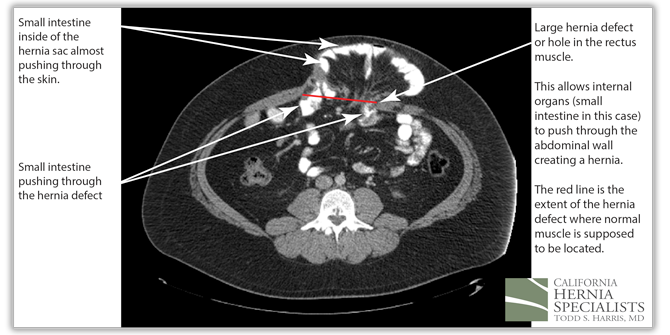
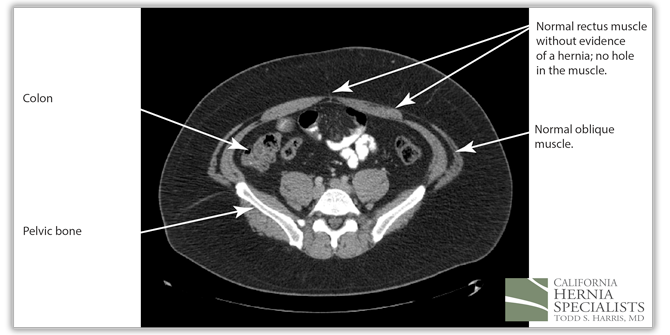
These 3 CT scan images show the patients muscle above the hernia where the muscle is normal, at the level of the hernia, and then below the hernia again where the muscle is normal.
In the images below we compare the pre-operative photos to the post-operative photos taken just 2 weeks after his surgery.

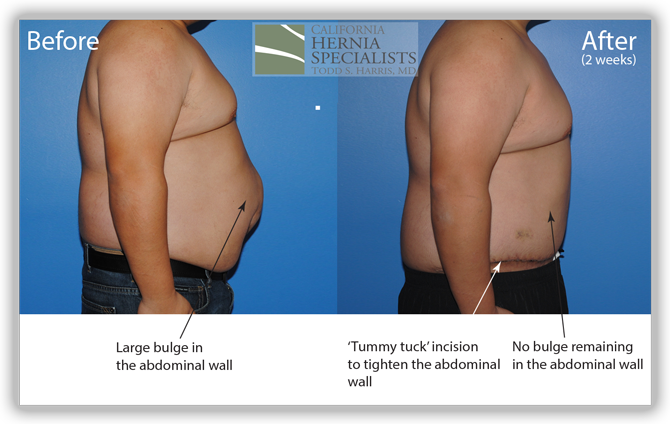
The patient continued to lose weight after his surgery. He was followed for 6 months and did very well throughout this time returning to normal activities after about 4-6 weeks.
Click here to close3. Recurrent incisional hernia in a 54 year old male after cancer surgery.
A 54 year old gentleman had a small cancer removed from his stomach several years prior. After that initial surgery he did well, until he felt a lump. His surgeon diagnosed him with an incisional hernia and he was taken back to the operating room for repair of this hernia.
Despite the fact that the surgeon used a small mesh, after only a few months the patient felt a bulge in the same area. The surgeon then re-operated and placed a larger mesh. Almost immediately after this surgery, the patient felt a recurrent lump and fullness in the incision. He presented to California Hernia Specialists for evaluation.
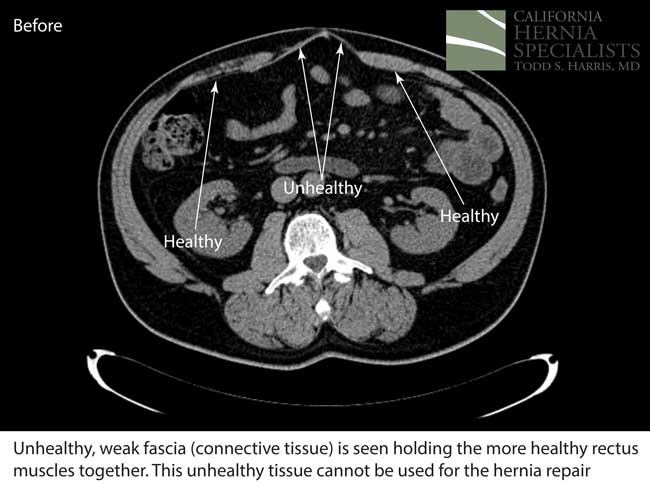
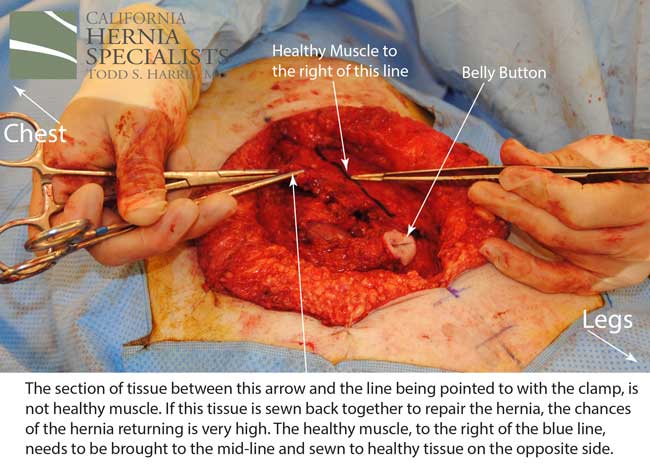
This initial CAT scan image shows why the hernia repair continued to fail. There is very weakened muscle in the middle of the abdomen with most of the healthy muscle several inches away on each side. More likely than not, the prior surgeon simply sewed the meshes into this unhealthy layer of fascia instead of bringing together the normal, healthy muscle.
Click here for more images and pictures
After this CT scan was obtained, a lengthy discussion with the patient was undertaken to explain the reasons for the prior hernia repair failures, and to explain all the options. By simply returning to the operating room and putting in more mesh, and sewing it to unhealthy muscle, we would not be actually repairing the hernia.
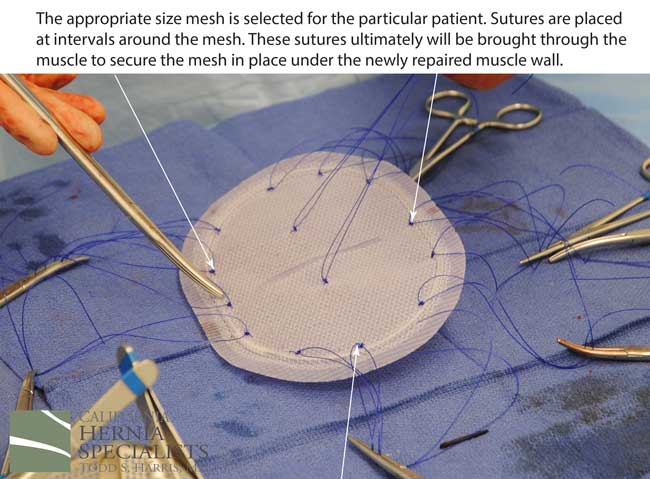
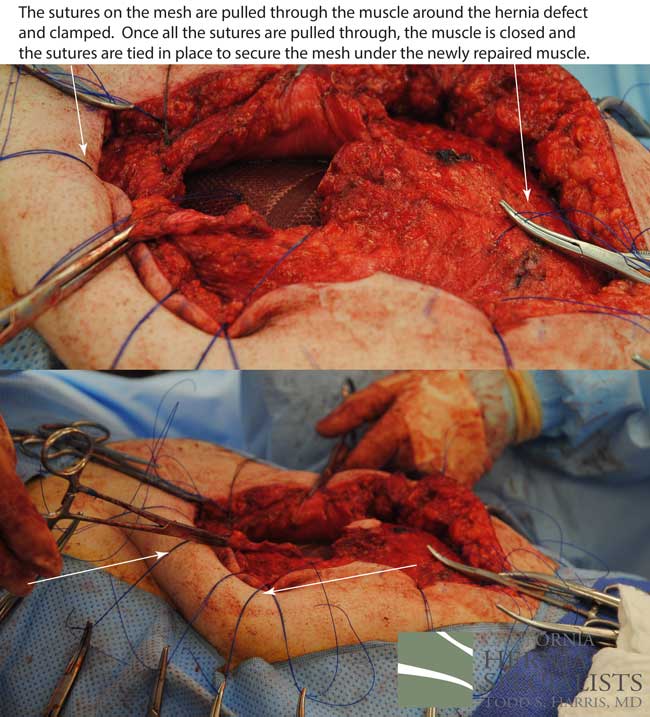
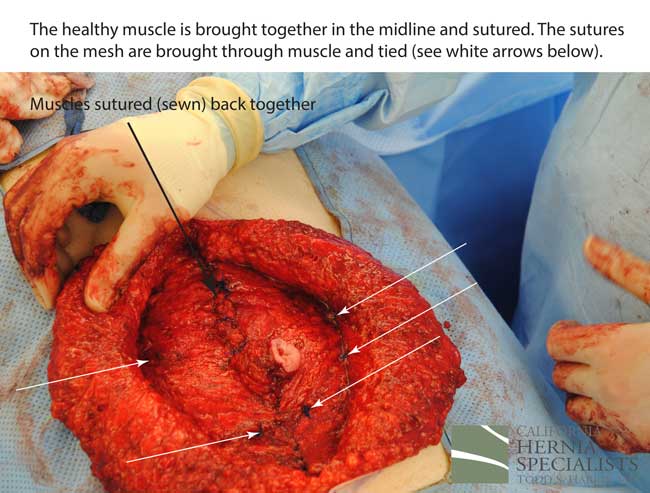
The more complete approach would be to bring healthy muscle together at the mid-line. Only after the muscle is repaired completely, can a mesh be used to SUPPORT the muscle repair. Meshes should not be considered a bridge from healthy muscle to healthy muscle. Instead mesh should be used as a reinforcement of a correct hernia repair.
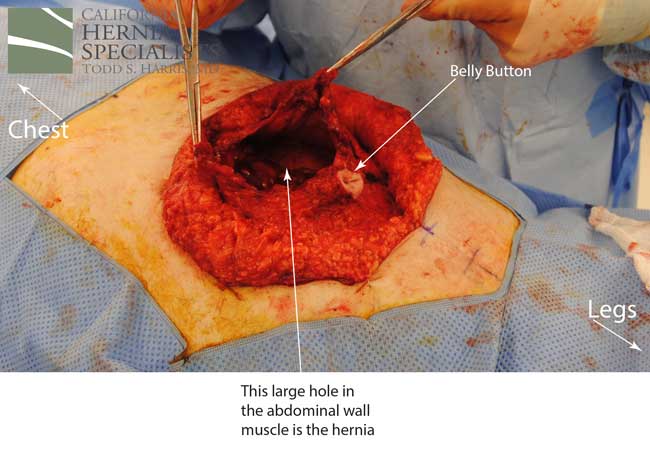
This technique requires more surgical time, recovery time, and usually several days in the hospital.However, this patient chose to proceed with the open hernia repair. Below are some of the pictures from his surgery as well as post operative CT scan image and photos of the patient.



 Click here to close
Click here to close 














