What to Expect on Your Hernia Surgery Day: Preparation, Process, and Recovery
Dr. Todd Harris walks patients through the timeline of their surgery day, including preparation, arrival, the surgical process, and recovery requirements.
Preparation, Process, and Recovery
Surgery can be an anxiety-provoking experience, but it doesn’t have to be. In this video, Dr. Todd Harris walks you through exactly what to expect before, during, and after your hernia repair at California Hernia Specialists. From managing medications like blood thinners and aspirin 5 days out to the specific “NPO” (fasting) rules, we ensure you are fully prepared before you even arrive. Learn about our sedation protocols, the typical one-hour surgery timeline, and how we involve family members in the recovery process to make your experience as comfortable and stress-free as possible.
Specialist Overview: The Surgical Experience
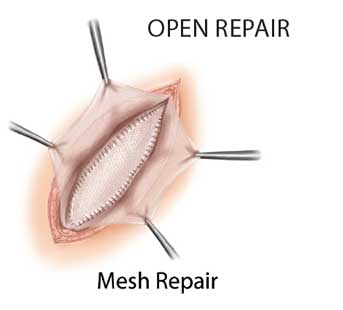
Hernia surgery is an elective procedure designed to repair a defect in the abdominal wall and prevent future complications. Modern hernia surgery has evolved into a highly specialized field, focusing on “anatomic restoration” to ensure the repair is tension-free and durable. The surgical process involves identifying the hernia sac, reducing the contents back into the abdominal cavity, and reinforcing the weak area using either the patient’s own tissue or specialized prosthetic mesh.
- Anesthesia & Safety: Most repairs are performed under a combination of local anesthesia and intravenous sedation (“twilight sleep”), which reduces the risks associated with general anesthesia.
- Recovery Timeline: In a high-volume setting, patients typically return home within hours of the procedure and can resume light daily activities within 24 to 48 hours.
- The Goal of Repair: To provide a permanent solution that restores core integrity while minimizing the risk of chronic postoperative pain.
A National Standard for Surgical Excellence
At California Hernia Specialists, we perform over 500 hernia repairs annually, maintaining a “Center of Excellence” standard. Under the leadership of Dr. Todd Harris, an 11-year OCMA Physician of Excellence (2015–2025), our surgical protocols are anchored in the latest research. This includes our role as Principal Investigator for the NOPIOIDS trial (NCT05929937) and our published outcomes on specialized pain management (PMID: 39724506).
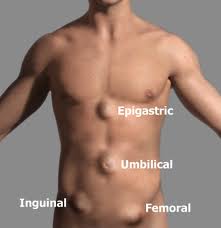
Hernia surgery can be described based on three specific categories:
- Where the hernia is located: inguinal hernias (groin hernia), umbilical hernias (belly button hernia), as well as less common incisional, femoral and ventral hernias
- How the hernia is repaired: traditional open repair or laparoscopic
- They can be further classified as: unilateral (one side of the body), bilateral (both sides of the body), or recurrent (after a prior surgical repair)
Open versus Laparoscopic Hernia Surgery
The two major types of hernia surgery are traditional open surgery, and laparoscopic surgery. No one approach is suitable for every patient. Patients with certain types of hernias may benefit from open hernia surgery while another similar patient may need laparoscopic hernia repair. The size of the hernia, the location, and whether it is unilateral or bilateral influences the best approach. Patients can read our:
- ‘Open Surgery‘ page
- ‘Laparoscopic Surgery‘ page
- ‘Comparison of Open & Laparoscopic Hernia Surgery‘ page
to read the pro’s and con’s of each type of surgery, as well as compare them to each other.
Tension Vs. Tension-Free Hernia Repair
The term ‘tension’ or ‘tension-free’ is commonly used when describing a particular hernia surgery. Hernias are caused by a weakening of the abdominal muscles which over time develops into a true hole. For patients who desire a no mesh repair, the muscles surrounding the hernia defect are sewn back together to close the hernia. This pulling together of the muscles creates tension which his why primary (no mesh) repairs are considered ‘tension repairs’.
In many patients, whether due to the size of the hernia or the patient, it’s not advisable for a surgeon to simply pull the muscles back together. In those cases, most hernia specialists today utilize a mesh to help strengthen the muscles and the hernia repair. When using a mesh, the muscles themselves are often not sewn together limiting the tension on the tissues providing a ‘tension free’ repair. Instead, a mesh is placed over or under the hole in the muscle to prevent anything from pushing through the abdominal wall.
Mesh Versus No Mesh Hernia Repairs
While a no mesh hernia repair is an option for some patients, many others will strongly benefit from the use of a mesh. Some patients have heard or read negative information about mesh surgery. However, the unbiased government agency The National Institutes of Health performed a study of whether mesh should or should not be used for hernia surgery and found that in the vast majority of patients, a mesh is the recommended approach to repairing a hernia. They also found that in the right hands, the use of a mesh causes little if any additional risks to the patient. Read the article by clicking on the logo below:

Patients can read more on our ‘Truths About Hernia Mesh‘ page.
Choosing a Non-Mesh Repair: Patient Autonomy and Safety
While modern surgical mesh is statistically the most durable option, Dr. Todd Harris understands that for patients with autoimmune diseases or foreign body sensitivities, a tissue-only repair may be the preferred choice. By weighing personal health priorities against recurrence rates, we help you decide on a specialized plan that minimizes inflammatory risk. Dr. Todd Harris discusses the clinical benefits of tissue-only (non-mesh) hernia repair for patients with autoimmune concerns or foreign body sensitivities.
Dr. Harris continues to advance open surgery outcomes as the Principal Investigator for the NOPIOIDS trial (NCT05929937), focusing on narcotic-free recovery for both open and laparoscopic repairs.
Mesh Safety: Separating Fact from Fear
We understand that headlines about hernia mesh can be alarming. In this video, Dr. Todd Harris explains why the data supports the use of modern, lightweight mesh for the majority of patients. By using the ‘tension-free’ repair method—think of patching a hole in old jeans rather than pulling the fabric tight—we can drastically reduce the risk of recurrence. Our practice uses only the most advanced, biocompatible materials to ensure your repair is strong, flexible, and permanent.
Choosing a Hernia Surgeon
When making your final decision on hernia care, it is vital to evaluate three things: Surgeon Priority, Surgical Volume, and Facility Specialization. At California Hernia Specialists, Dr. Todd Harris focuses exclusively on hernias. By combining high-volume experience with a dedicated outpatient center and a staff trained specifically in hernia recovery, we minimize complication rates and get you back to 100% as safely as possible.
Hernia Surgery Costs and Insurance
Navigating the financial aspect of surgery shouldn’t be a hurdle to your health. Dr. Todd Harris explains how our office manages insurance verification for PPO plans and offers transparent cash pricing and payment plans for self-pay patients. From your initial consultation through diagnostic tests like EKGs and bloodwork, we provide a clear path to getting your hernia fixed.
How Can You Minimize Recurrent Hernias and Complications?
Patients often cannot affect their risk of developing a primary (first time) hernia. However, patients can minimize the chances of having a recurrent hernia or chronic postoperative pain by choosing a surgeon who performs a high volume of hernia surgeries. Just like no one would want to fly with a pilot who only flies a few times a month, a surgeon who operates on hernias infrequently cannot provide leading care. In addition, finding a surgeon who publishes their surgical volume and outcomes data for future patients to review will ensure that you are choosing someone who can provie the outcome that you are looking for in a surgeon. Patients can read about our Hernia Patient Outcome Data here, or about recurrent hernias and complications from hernia surgery on our ‘Complications of Hernia Surgery‘ page along with how our center minimizes these risks.
What to Expect From Hernia Surgery
We know that visiting a doctor can be an uneasy experience. Most patients will (hopefully) only visit a few surgeons in their life. Not knowing what to expect and not knowing anything about the surgeon you are seeing can cause anxiety! We are extremely proud of our patient centered care and the experience our patients have with us. That’s why we encourage our past patients to give feedback about our practice and Dr. Harris. Whether this feedback is in the form of a letter, or on HealthGrades and Yelp, our past patients ease the anxiety of our future patients. In the videos below, some of our past patients discuss what their experience was like with hernia surgery at our center.