What is a Ventral Hernia? Location, Repair & Recovery | Dr. Todd Harris
Dr. Todd Harris defines Ventral Hernias, explaining their specific location in the upper abdomen (epigastric region), surgical repair with mesh, and recovery expectations.
Ventral vs. Umbilical: Understanding the Difference
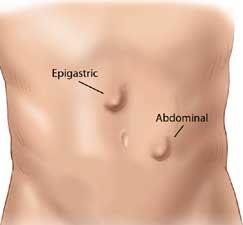
Patients often confuse Ventral and Umbilical hernias because they both occur in the center of the abdomen. In this video, Dr. Todd Harris clarifies the difference based on anatomy. While an Umbilical hernia is at the navel, a Ventral (or Epigastric) Hernia occurs higher up—specifically in the midline between the belly button and the ribcage. Understanding this location is key to diagnosis, though the repair techniques (outpatient surgery with mesh reinforcement) are often similar.
Specialist Overview
Ventral hernias are openings in the abdominal wall muscles that allow tissue or organs to push through. These often occur at the site of a previous surgical incision (incisional hernia) or as a primary defect in the midline of the abdomen. Large or complex ventral hernias often require abdominal wall reconstruction to restore functional core strength.
- Pathology: Common in patients with weakened tissue from previous surgeries, obesity, or heavy physical strain.
- Repair Methodology: Utilization of laparoscopic tension-free techniques to close and reinforce the defect while minimizing surgical trauma to the abdominal wall.
- Outcome Focus: Precise placement of reinforcement to prevent recurrence while ensuring the patient retains a full range of motion.
Proven Clinical Leadership
Specializing in ventral hernia repairs, Dr. Harris is recognized by the American Hernia Society for his expertise in surgical quality. His evidence-based approach to ventral repair is documented in his peer-reviewed research on postoperative prescribing patterns (PMID: 39724506) and his role as Principal Investigator for the NOPIOIDS clinical trial (NCT05929937).
Hernia Types – Ventral -The Basics
These types of hernias are similar to all other hernias in that they form due to weakening of the abdominal muscles. These hernias are located between the belly button or navel, and the lower part of the breast bone. Repair of these hernias is very common and can be done with open surgery or laparoscopic surgery techniques.
Symptoms of a ventral or epigastric hernia
Like most other hernias, pain in the abdomen is one of the most common symptoms. Also, due to the fat and intestines pushing through the hernia, a bulge can often form under the skin. This bulge can get bigger and smaller depending on what is in the hernia.
Over time, if the hernia gets large enough, the intestine can get permanently trapped, which can lead to damage to the intestine, as well as other symptoms like nausea, vomiting, and constipation.
Read more about symptoms our ‘Hernia Symptoms‘ page.
How are ventral hernias repaired?
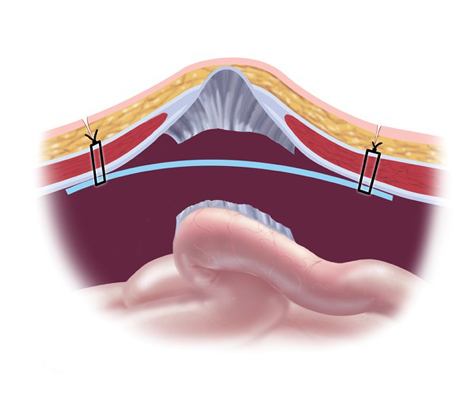
Ventral hernias, epigastric hernias, as well as several other, are excellent candidates for laparoscopic hernia repair since the hole is usually large and is surrounded by weakened abdominal muscles.. Similar to an inguinal hernia, a camera is placed through the muscle into the abdomen along with two smaller punctures for the operating instruments. From there, any scar tissue between the intestine and the hernia is cut allowing complete exposure of the hole.
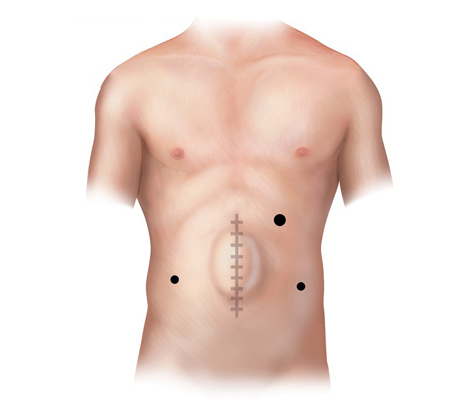
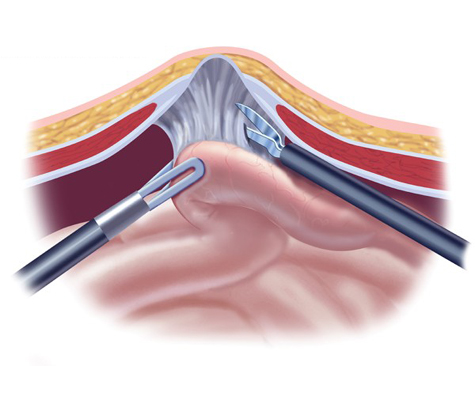
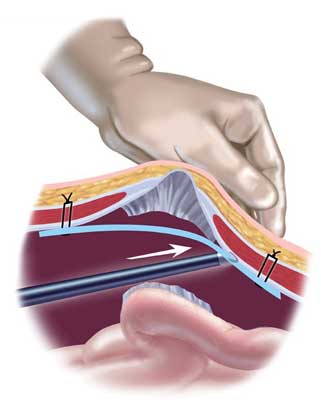
A hernia mesh is rolled and placed through one of the laparoscopic ports into the abdomen. From there, it is pulled up against the muscle surrounding the hernia with stitches (sutures). Once the mesh is secured in place with about 4 sutures, a special stapling device is used to further fix the mesh to the healthy muscle.
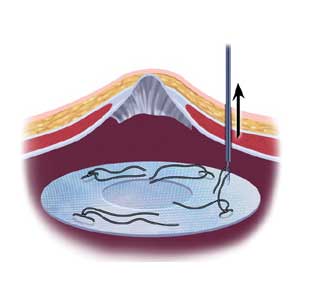
We perform a tension free mesh repair technique utilizing the latest mesh available. Mesh helps prevent recurrences after the hernia repair by strengthening the muscle around the hernia defect. Learn more about hernia mesh on our ‘Truths About Hernia Mesh‘ page.
Repairing “Swiss Cheese” Defects: The IPOM-Plus Technique
Incisional hernias often present not as a single hole, but as multiple small defects resembling Swiss cheese, frequently complicated by muscle separation (diastasis). In this video, Dr. Todd Harris demonstrates why simply placing a mesh patch isn’t enough. We utilize the IPOM-Plus technique: first, we use a suture passer to physically close the muscle defects and diastasis, restoring the abdominal wall’s function. Only then do we place the mesh reinforcement (using the precise Echo Positioning System) to prevent recurrence.
Mesh Safety: Separating Fact from Fear
We understand that headlines about hernia mesh can be alarming. In this video, Dr. Todd Harris explains why the data supports the use of modern, lightweight mesh for the majority of patients. By using the ‘tension-free’ repair method—think of patching a hole in old jeans rather than pulling the fabric tight—we can drastically reduce the risk of recurrence. Our practice uses only the most advanced, biocompatible materials to ensure your repair is strong, flexible, and permanent.














