Laparoscopic TEP Hernia Repair: GoPro External & Internal Views | Dr. Todd Harris
A dual-view surgical walkthrough of a bilateral TEP inguinal hernia repair, showing synchronized external GoPro footage and internal laparoscopic views.
Specialist Overview: Minimally Invasive “Keyhole” Repair
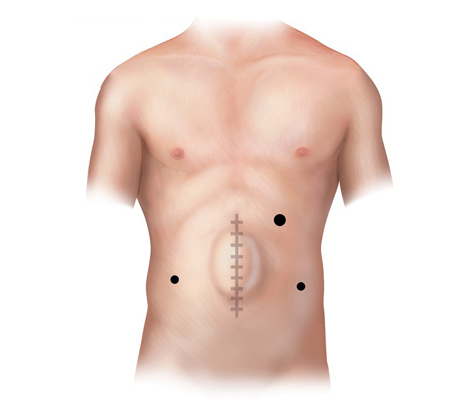
Laparoscopic hernia surgery is a minimally invasive “posterior” approach that utilizes a high-definition camera and specialized instruments to repair a hernia from the inside. Instead of a single larger incision, the surgeon creates three small incisions (typically 5-10mm) to place a reinforcement bridge behind the abdominal wall defect. This technique is particularly advantageous for bilateral (double) hernias and recurrent hernias where previous open surgery has left significant scar tissue.
- TAPP & TEP Techniques: We utilize both Transabdominal Preperitoneal (TAPP) and Totally Extraperitoneal (TEP) approaches, depending on the patient’s specific anatomy and surgical history.
- Rapid Recovery: Because there is minimal disruption to the overlying skin and muscle, laparoscopic patients often experience less immediate post-operative pain and a faster return to physical exercise.
- Bilateral Advantage: Both the left and right sides can be repaired through the same three small ports, avoiding the need for multiple open incisions.
Advanced Technology, Proven Results
At California Hernia Specialists, we integrate the most advanced minimally invasive technology with the rigorous safety standards of a high-volume center. Led by Dr. Todd Harris, an 11-year OCMA Physician of Excellence (2015–2025), our laparoscopic protocols are optimized for opioid-free recovery (NCT05929937) and are backed by our published research on surgical outcomes (PMID: 39724506).
Laparoscopic Hernia Surgery Repair – Inguinal
A laparoscopic inguinal hernia requires a 1-2cm incision at the belly button, and two smaller punctures below the umbilicus. The belly button incision allows the camera to view the inside of the abdomen and the two smaller punctures are for the operating instruments.
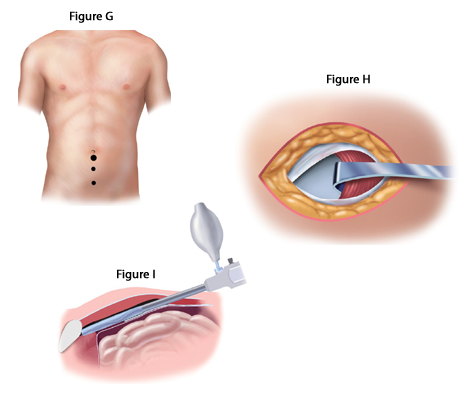

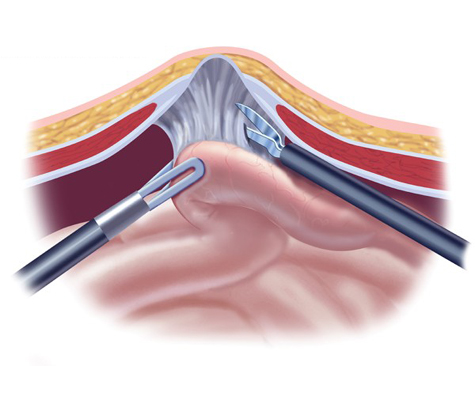
To begin, a trocar is placed at the umbilicus and gas is inflated to separate the peritoneum, or the lining of the abdomen, from the overlying muscle. Once this space is created, a camera is placed under the muscle to view the hernia.
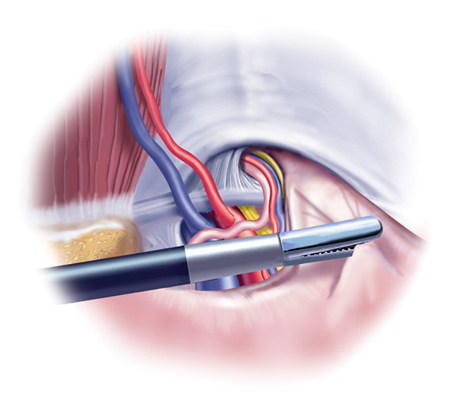
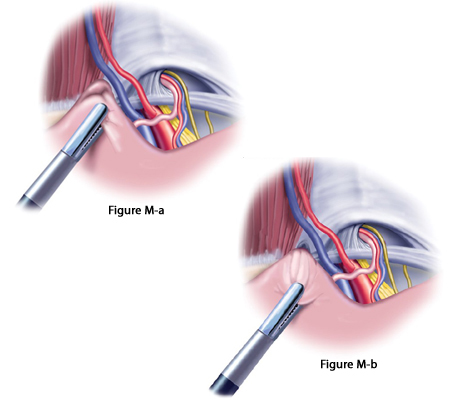
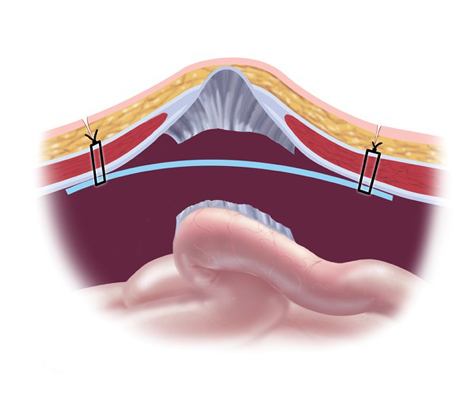
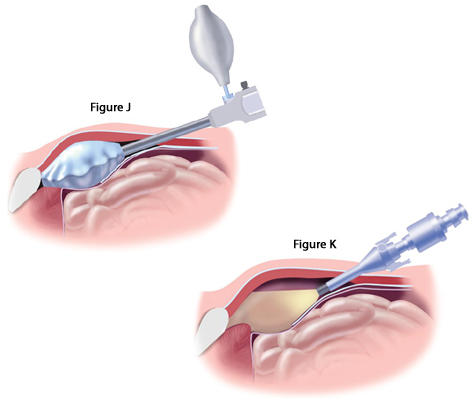 The hernia is then pulled back into the abdomen from it’s hole in the muscle. This hole can either be lateral to the blood vessels (indirect inguinal hernia, left below) or towards the middle from the blood vessels (direct inguinal hernia, right below). Regardless, the surgery is the same; once the hole is found, a small mesh is placed under the muscle to reinforce the hernia defect.
The hernia is then pulled back into the abdomen from it’s hole in the muscle. This hole can either be lateral to the blood vessels (indirect inguinal hernia, left below) or towards the middle from the blood vessels (direct inguinal hernia, right below). Regardless, the surgery is the same; once the hole is found, a small mesh is placed under the muscle to reinforce the hernia defect.
Skin-to-Skin” Walkthrough: The Surgeon’s Perspective
Patients often ask where the instruments go and how we navigate during laparoscopic surgery. In this special ‘Dual-View’ video, Dr. Todd Harris synchronizes external footage of the operating field with the internal camera view. You will see the precise placement of trocars, the dissection of the pre-peritoneal space, and the repair of bilateral direct hernias. This level of transparency helps demystify the TEP (Totally Extraperitoneal) technique, showing exactly how we reinforce the abdominal wall without entering the main abdominal cavity
Complex Case: Laparoscopic Scrotal Hernia Repair
When an inguinal hernia is neglected, it can descend into the scrotum, adhering to the spermatic cord structures. In this video, Dr. Todd Harris demonstrates the delicate laparoscopic dissection required to retrieve these ‘scrotal hernias.’ You will see exactly how we identify and protect the vas deferens and testicular vessels while reducing the hernia sac. Dr. Harris also points out the ‘Triangle of Pain’—the area containing the lateral femoral cutaneous and genitofemoral nerves—to show how we place mesh fixation tacks safely to avoid chronic post-operative pain.
Bilateral Repair: Fixing Both Sides in One Surgery
One of the primary advantages of the laparoscopic approach is the ability to repair bilateral hernias (both left and right) through the same small incisions. In this video, Dr. Todd Harris walks you through a complex case involving a Direct Hernia on the right side—where the weakness is in the floor of the inguinal canal—and an Indirect Hernia on the left. You will see how we navigate critical structures like the iliac vessels (often called the ‘Triangle of Doom’) and overlap the mesh in the midline to ensure complete reinforcement of the abdominal wall.
Laparoscopic Hernia Surgery Repair – Ventral/Incisional
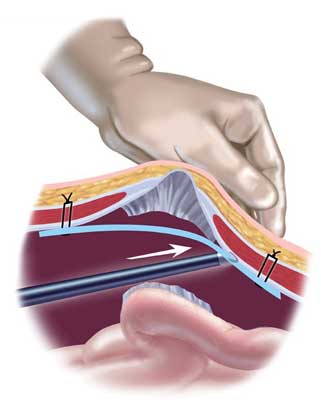
Ventral hernias, epigastric hernias, recurrent umbilical hernias, as well as several other, are excellent candidates for laparoscopic hernia repair. Similar to the inguinal hernia, a camera is placed through the muscle into the abdomen along with two smaller punctures for the operating instruments. From there, any scar tissue between the intestine and the hernia is cut allowing complete exposure of the hole.
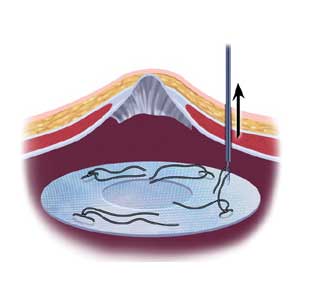
A hernia mesh is rolled and placed through one of the laparoscopic ports into the abdomen. From there, it is pulled up against the muscle surrounding the hernia with stitches (sutures). Once the mesh is secured in place with about 4 sutures, a special stapling device is used to further fix the mesh to the healthy muscle.
Patients should read our ‘Comparison of Open & Laparoscopic Surgery‘ page to read the pro’s and con’s of open versus laparoscopic surgery.
Laparoscopic Ventral/Incisional Hernia Repair Cases
The following two patients had incisional hernias which came back after a prior surgical repair (recurrent incisional hernias). Both were done at large university hospitals and both recurred within months after having their surgery. We treated both patients with laparoscopic surgery after discussions with the patients about their desires and expectations for after the surgery. Some patients will benefit from laparoscopic repair, while some might benefit from an open approach.
1. Laparoscopic repair of recurrent incisional hernia in a 74 year old doctor.
A 74 year old physician had a large pelvic tumor removed which was non cancerous. She developed a hernia 2 years after her surgery and underwent a laparoscopic incisional hernia repair at a large University Hospital in Southern California. Weeks after her surgery, she noticed a recurrent bulge in the lower part of her abdomen.
She presented to California Hernia Specialists for evaluation and treatment. On examination she had a 1-2 inch bulge in the lower abdomen, just above her pubic bone. This recurrent incisional hernia was painful when she exercised and while she was at work. We offered her laparoscopic recurrent incisional hernia repair.
Repairing “Swiss Cheese” Defects: The IPOM-Plus Technique
Incisional hernias often present not as a single hole, but as multiple small defects resembling Swiss cheese, frequently complicated by muscle separation (diastasis). In this video, Dr. Todd Harris demonstrates why simply placing a mesh patch isn’t enough. We utilize the IPOM-Plus technique: first, we use a suture passer to physically close the muscle defects and diastasis, restoring the abdominal wall’s function. Only then do we place the mesh reinforcement (using the precise Echo Positioning System) to prevent recurrence.
2. Hernia in a 30 year old woman after endometriosis surgery and c-section.
This patient had several surgeries for endometriosis and c-sections. After one of her surgeries she developed pain in the lower abdomen and a bulge. The bulge would get bigger and smaller, and sometimes extend down to the right labia. She had pain with most activities including simple tasks like standing and sitting.

She had a laparoscopic hernia repair previously, but the mesh wasn’t placed low enough to cover the entire hernia defect, or the hole in the muscle. She presented to us for a second opinion and further treatment. Her small intestine was stuck in the hole at the beginning of the surgery and had to be pulled out prior to repairing the defect. A ‘tension free’ repair (see below) was performed.
Tension Vs. Tension-Free Hernia Repair
The term ‘tension’ or ‘tension-free’ is commonly used when describing a particular hernia surgery. Hernias are caused by a weakening of the abdominal muscles which over time develops into a true hole. For patients who desire a no mesh repair, the muscles surrounding the hernia defect are sewn back together to close the hernia. This pulling together of the muscles creates tension which his why primary (no mesh) repairs are considered ‘tension repairs’.
In many patients, whether due to the size of the hernia or the patient, it’s not advisable for a surgeon to simply pull the muscles back together. In those cases, most hernia specialists today utilize a mesh to help strengthen the muscles and the hernia repair. When using a mesh, the muscles themselves are often not sewn together limiting the tension on the tissues providing a ‘tension free’ repair. Instead, a mesh is placed over or under the hole in the muscle to prevent anything from pushing through the abdominal wall.
Choosing a Non-Mesh Repair: Patient Autonomy and Safety
While modern surgical mesh is statistically the most durable option, Dr. Todd Harris understands that for patients with autoimmune diseases or foreign body sensitivities, a tissue-only repair may be the preferred choice. By weighing personal health priorities against recurrence rates, we help you decide on a specialized plan that minimizes inflammatory risk. Dr. Todd Harris discusses the clinical benefits of tissue-only (non-mesh) hernia repair for patients with autoimmune concerns or foreign body sensitivities.
Dr. Harris continues to advance open surgery outcomes as the Principal Investigator for the NOPIOIDS trial (NCT05929937), focusing on narcotic-free recovery for both open and laparoscopic repairs.
Mesh Safety: Separating Fact from Fear
We understand that headlines about hernia mesh can be alarming. In this video, Dr. Todd Harris explains why the data supports the use of modern, lightweight mesh for the majority of patients. By using the ‘tension-free’ repair method—think of patching a hole in old jeans rather than pulling the fabric tight—we can drastically reduce the risk of recurrence. Our practice uses only the most advanced, biocompatible materials to ensure your repair is strong, flexible, and permanent.
Our Approach
Our office specializes in the surgical repair for all hernia types. We provide patients with the full spectrum of treatment options from open no mesh hernia repairs to advanced minimally invasive laparoscopic techniques. Dr. Harris and our team perform over 500 hernia repairs each year making us the busiest center on the West Coast, and one of the top 3 in the country.
For over 10 years we have partnered with the Abdominal Core Health Quality Collaborative (ACHQC) to track the outcome of every surgery we perform. Year over year, our nationally leading outcome data shows a lower chance of hernia recurrence and a lower risk of developing chronic pain – data which we actively publish on our website. Our commitment to cutting edge hernia care, the full spectrum of surgical options, as well as research and transparency in our data, helps ensure you will have the best outcome after your hernia surgery.














