
Not infrequently, California Hernia Specialists sees unique cases which present in patients with a complicated history, or with numerous previous surgeries. Although these cases can be challenging, they are also interesting and rewarding since patients who often are told there is nothing that can be done and are in chronic pain, can be treated. Below is a short list of recent case highlights at California Hernia Specialists. Each case has corresponding photos, videos and CAT scan images to help explain what was done during the surgery.
Complicated Hernia Repairs
Complicated hernias are unfortunately not uncommon in todays health care environment. Patients can often have difficulty obtaining health insurance, or may just be scared of seeing a surgeon. Over time their hernia gets larger until the point that they come to our center with what we describe as a complicated hernia.
Although there is no formal medical definition for a ‘complicated’ hernia, there are some general characteristics. Complicated hernias are those that may not be able to be pushed back into the abdominal cavity, and are thus incarcerated. Men with inguinal hernias, or groin hernias, which extend into the scrotum become more complicated to repair. Some patients who have already had prior hernia repair, or who have large incisional hernias from a prior surgery, are also considered to be more complicated.
Complicated Hernia Repairs
Dr. Todd Harris discusses some of the challenges and possible complications when doing surgery on patients with large, complicated hernias.Recent Case Highlights
Below is a list of both complicated, and interesting cases that we have done at California Hernia Specialists. Click any of the case titles to expose the detailed content and associated pictures.
1. Two recurrent umbilical hernias in a 27 year old patient.
This patient had been operated on two previous times by an outside surgeon. The first surgery was done without mesh. After it recurred almost immediately, the same surgeon used a ‘large piece of mesh’ as was described by the patient and the operative report. Unfortunately shortly after this surgery, the bulge returned and the patient developed increasing pain.
The patient presented to California Hernia Specialists for a second opinion before returning for a third surgery. The patient underwent a physical exam and a CT scan to evaluate the size of the hernia. A number of options were presented to the patient and ultimately it was decided to treat him with an open recurrent umbilical hernia repair.
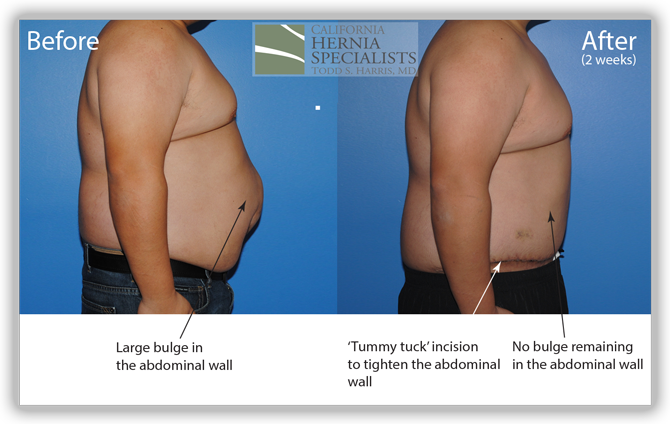
A ‘tummy tuck’ incision was used to help tighten and remove excess skin and the old scar. The old mesh had completely separated from the muscle and was stuck to the small intestines internally. Careful removal of the mesh was required to free the intestine from the hernia. The muscle was closed and a new piece of advanced mesh was placed under the muscle to reinforce the repair. The images below are from before and after his hernia surgery.
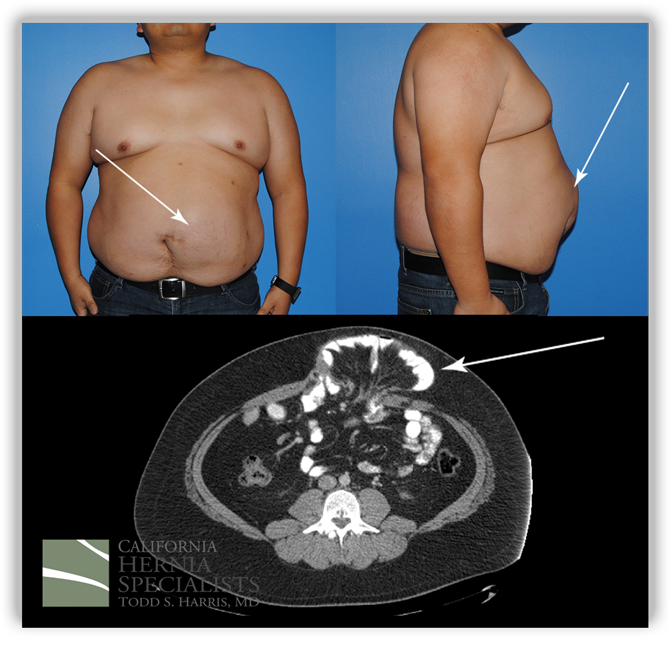
This image shows photos before his surgery along with the CT image corresponding to his hernia. The arrows point out the obvious hernia.
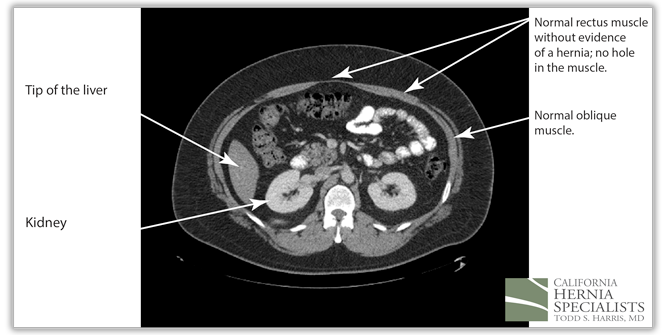
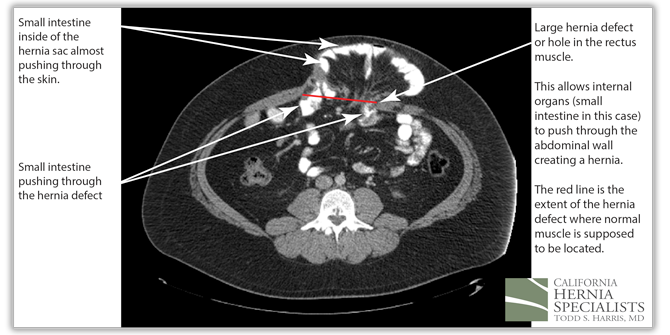
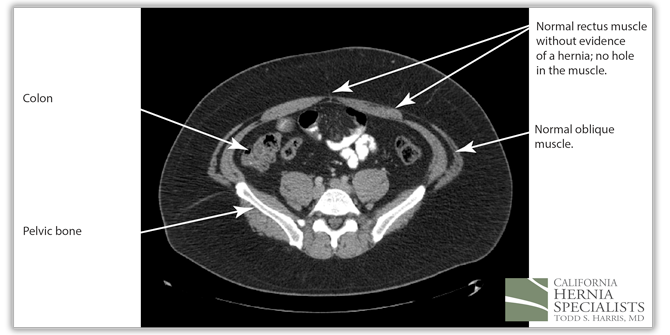
These 3 CT scan images show the patients muscle above the hernia where the muscle is normal, at the level of the hernia, and then below the hernia again where the muscle is normal.
In the images below we compare the pre-operative photos to the post-operative photos taken just 2 weeks after his surgery.

The patient continued to lose weight after his surgery. He was followed for 6 months and did very well throughout this time returning to normal activities after about 4-6 weeks.
Click here to close2. Recurrent incisional hernia after a pelvic tumor removal.
A 74 year old physician had a large pelvic tumor removed which was non cancerous. She developed a hernia 2 years after her surgery and underwent a laparoscopic incisional hernia repair at a large University Hospital in Southern California. Weeks after her surgery, she noticed a recurrent bulge in the lower part of her abdomen.
She presented to California Hernia Specialists for evaluation and treatment. On examination she had a 1-2 inch bulge in the lower abdomen, just above her pubic bone. This recurrent incisional hernia was painful when she exercised and while she was at work. We offered her laparoscopic recurrent incisional hernia repair.
The following video is a summary of her surgical procedure narrated by Dr. Harris.
Click here to close
3. Recurrent incisional hernia after cancer surgery.
A 54 year old gentleman had a small cancer removed from his stomach several years prior. After that initial surgery he did well, until he felt a lump. His surgeon diagnosed him with an incisional hernia and he was taken back to the operating room for repair of this hernia.
Despite the fact that the surgeon used a small mesh, after only a few months the patient felt a bulge in the same area. The surgeon then re-operated and placed a larger mesh. Almost immediately after this surgery, the patient felt a recurrent lump and fullness in the incision. He presented to California Hernia Specialists for evaluation.
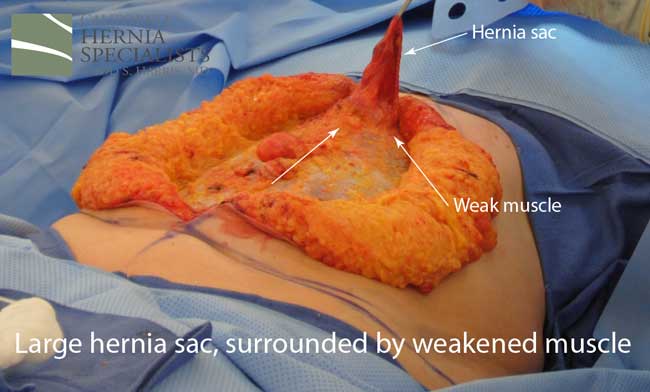
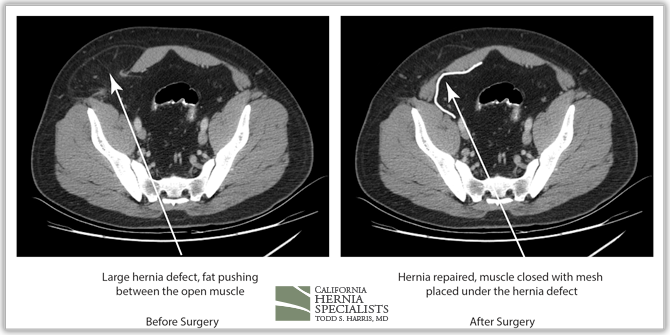
This initial CAT scan image shows why the hernia repair continued to fail. There is very weakened muscle in the middle of the abdomen with most of the healthy muscle several inches away on each side. More likely than not, the prior surgeon simply sewed the meshes into this unhealthy layer of fascia instead of bringing together the normal, healthy muscle.
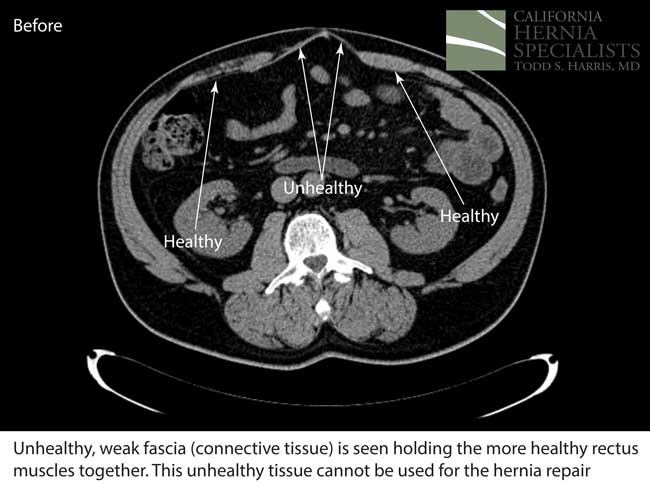
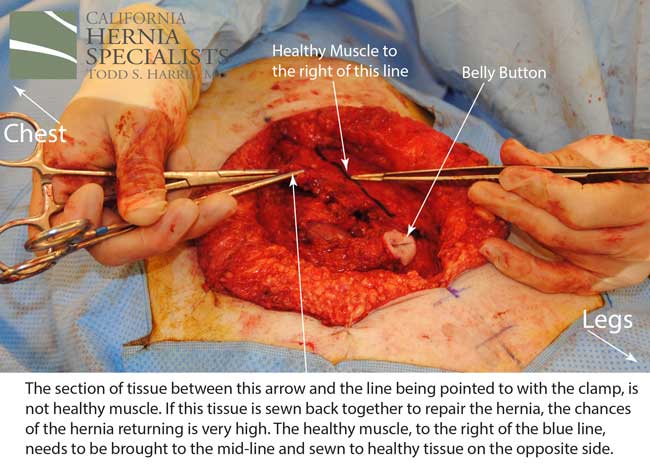
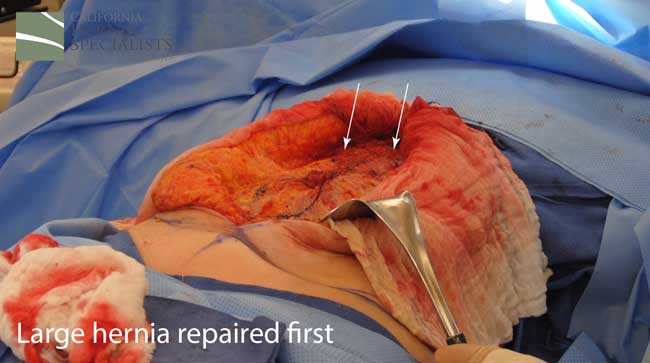
After this CT scan was obtained, a lengthy discussion with the patient was undertaken to explain the reasons for the prior hernia repair failures, and to explain all the options. By simply returning to the operating room and putting in more mesh, and sewing it to unhealthy muscle, we would not be actually repairing the hernia.
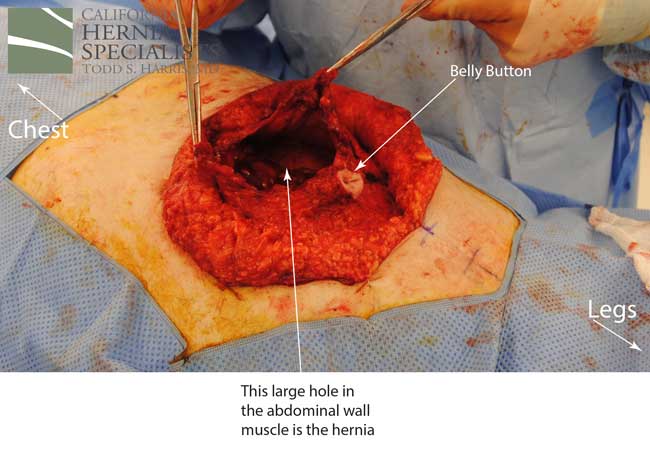
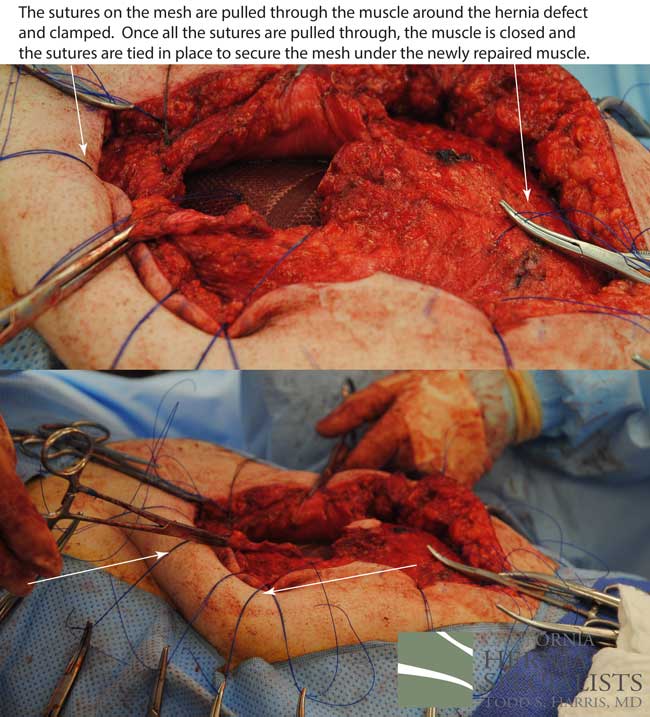
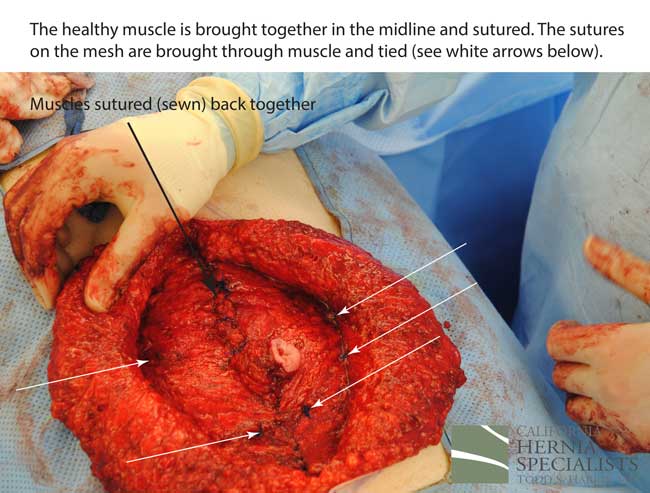
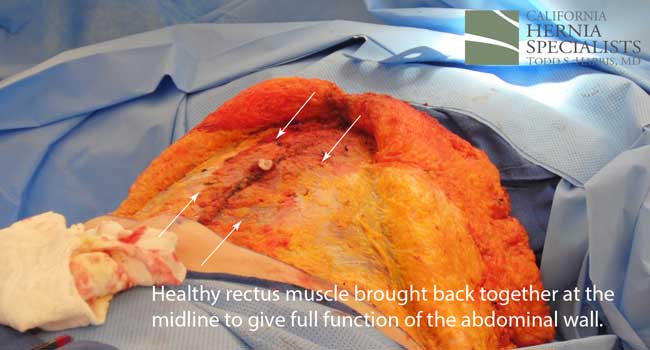
The more complete approach would be to bring healthy muscle together at the mid line. Only after the muscle is repaired completely, can a mesh be used to SUPPORT the muscle repair. Meshes should not be considered a bridge from healthy muscle to healthy muscle. Instead mesh should be used as a reinforcement of a correct hernia repair.
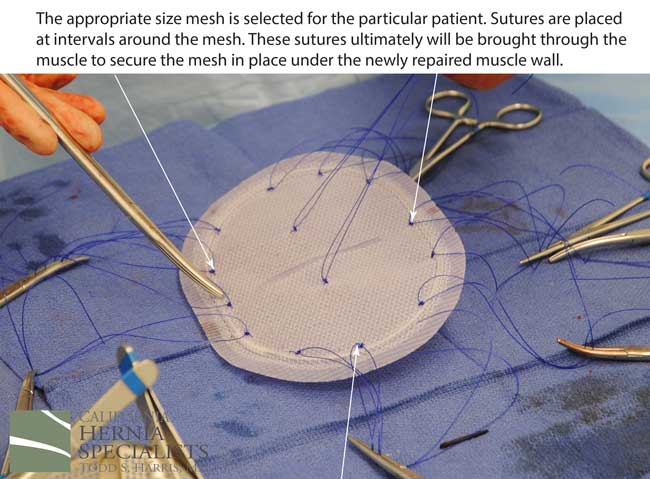
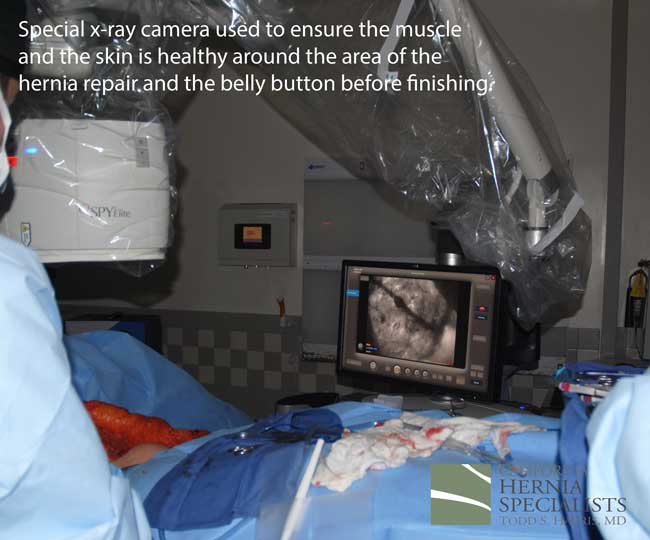
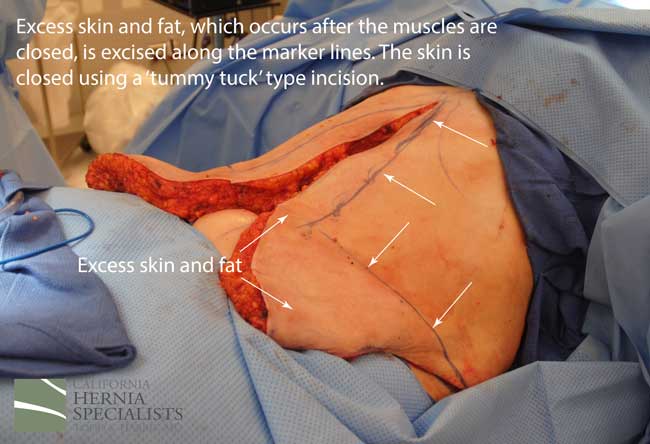
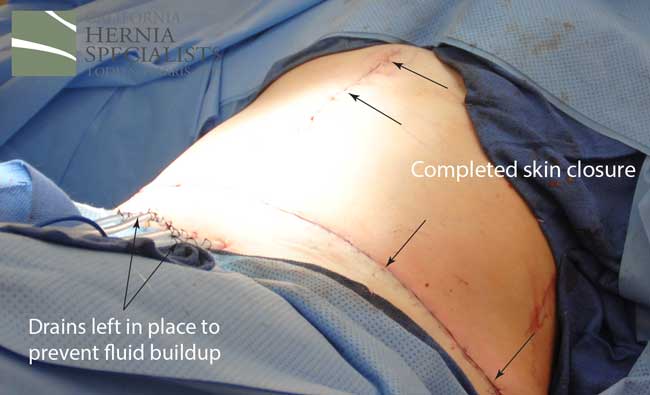
This technique requires more surgical time, recovery time, and usually several days in the hospital. However, this patient chose to proceed with the open hernia repair. Below are some of the pictures from his surgery as well as post operative CT scan image and photos of the patient.



 Click here to close
Click here to close
4. Recurrent incisional hernia after 3 prior repairs.
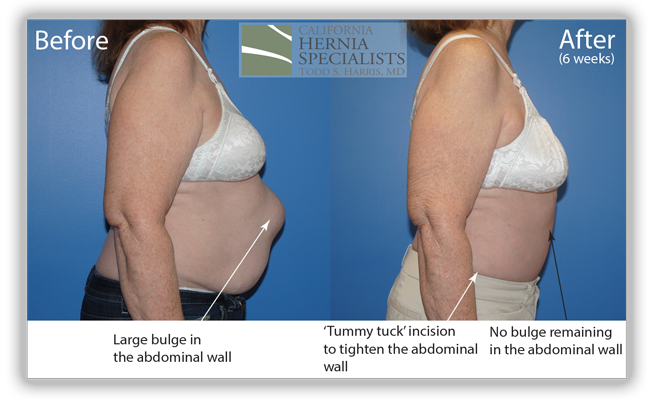
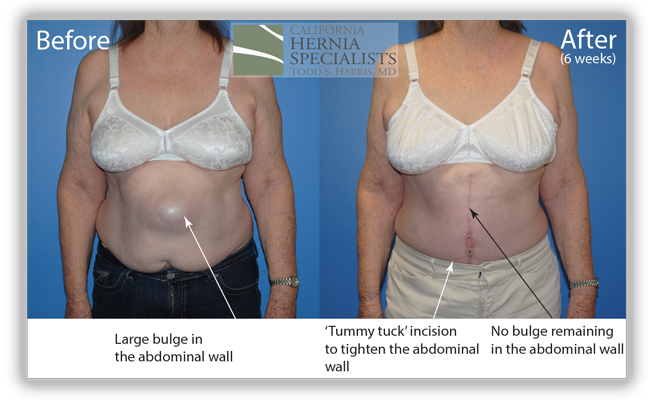
A 73 year old female had gallbladder surgery over 20 years ago. After that surgery she developed a small hernia at one of her incisions. This incisional hernia was repaired and she did well for over 10 years. Then the hernia returned and she underwent a second hernia repair. This only lasted for several years and the hernia returned. She had a 3rd attempt at hernia repair which only lasted several months before she noticed the bulge return.
She presented to California Hernia Specialists for evaluation and possible treatment. On examination it was clear that she had severe weakness of the muscles surrounding the hernia which was likely contributing to the repeated recurrences after her surgeries. Simply patching the hole in her muscle would not bring the healthy muscle back together and give her the best chance at preventing the hernia from returning. Thus laparoscopic hernia repair was not our recommendation.
Instead we discussed open hernia repair with a large incision to repair the damaged muscle and to remove excess skin and fat once the muscle was repaired. Below are a number of pictures including before and after photos, as well as photos taken during her surgery.

 Click here to close
Click here to close
5. Bladder trapped inside a groin hernia in a 48 year old male.
This 50 year old male patient developed a hernia over 10 years ago. Initially he didn’t have any symptoms from his hernia. However, over time, his symptoms got worse, including severe pain in his hernia area when his bladder was full. With more time, he noticed pain when he urinated, and with sexual activity.
He was seen by his primary care physician in Arizona who ordered a CAT scan. The scan showed the images below including a large portion of his bladder in the right hernia. He also had a moderate sized fat containing hernia in the left groin.
Due to the fact that he had hernias in both the left and right groins, he was an excellent candidate for laparoscopic surgical repair. However, the surgeon he was referred to in Arizona did not do laparoscopic hernia surgery so the patient sought treatment at California Hernia Specialists.
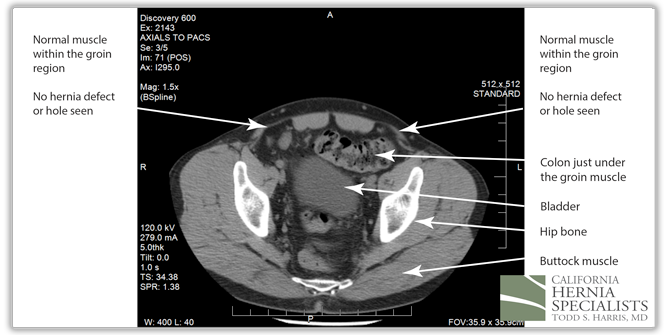
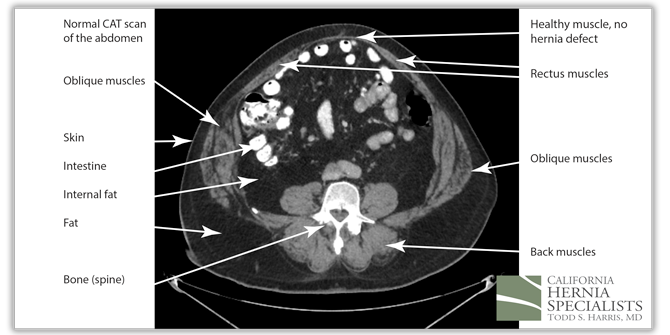
The CAT scan image above shows normal muscles of the abdominal wall with no evidence of a hole, or a hernia.
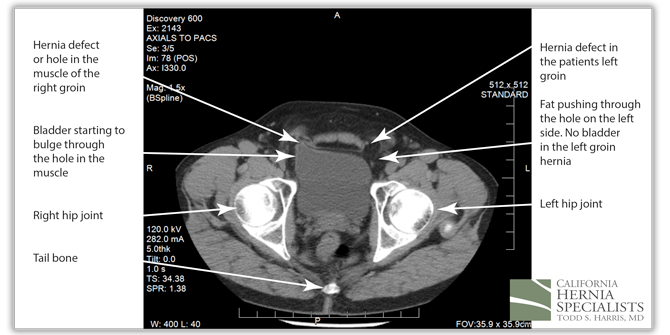
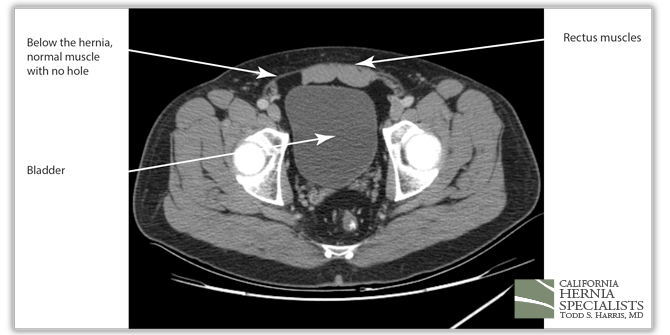
However, in this CAT scan image, there is a noticeable hole in the lower muscle wall, and the start of an inguinal hernia both on the left and the right side of the groin.
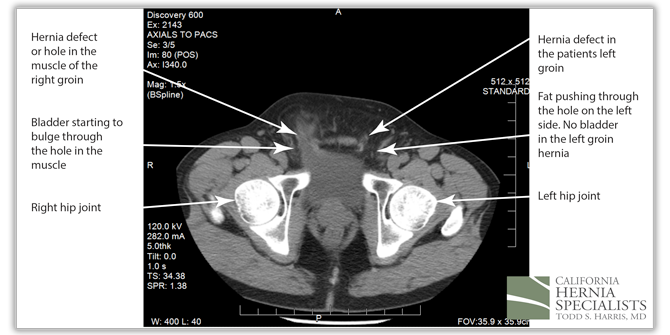
The bladder can be seen squeezing through the hole in the muscles within the patients right groin (left side of the CAT scan image). On the patients left side (right side of the image), there is only fat pushing through the hernia defect.
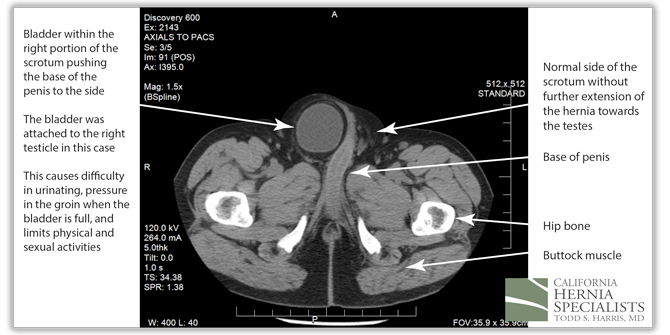
At the bottom of the hernia, the bladder on the right side was attached to the patients right testicle, and was pushing the base of the penis to the left side. When the patients bladder was full, he noticed severe pain in the groin, and difficulty urinating.
The patient underwent a laparoscopic bilateral inguinal hernia repair. During the surgery, the bladder was pulled out of the right groin hernia, and the fat was pulled out of the left hernia. Laparoscopic hernia mesh was placed to repair both groins. Due to the fact that the bladder was so close to the hernia repair, a bladder catheter was left in place for 2 weeks after the surgery to ensure complete healing.
Below is an 8 minute video recorded during this surgery. It is narrated by Dr. Harris and shows the technique used to remove the bladder from the hernia.
Click here to close
6. Recurrent incisional hernia after two c-sections in a 34 year old female.
This 35 year old female patient had several surgeries for endometriosis and 2 c-sections. After one of her surgeries she developed pain in the lower abdomen and a bulge. The bulge would get bigger and smaller, and sometimes extend down to the right labia. She had pain with most activities including simple tasks like standing and sitting.
Her primary care physician referred her to a large university hospital in the Inland Empire where she underwent a laparoscopic hernia repair. Initially after her surgery, she did well, but then quickly began experiencing the same bulge in the lower abdomen, and pain with standing or sitting.
Her primary physician then ordered an MRI scan to look for a residual cause of her bulge and her pain. The MRI showed fluid in the lower portion of the abdominal muscle, near the prior surgery. Her initial surgeon said that the fluid was normal post surgical fluid and that is would resolve over time. However, after months of pain and the inability to work, she presented to California Hernia Specialists for a second opinion.
At her consultation, we reviewed her MRI scan and examined her. It was clear that the fluid seen on the MRI was a recurrent incisional hernia in the muscle, despite her having had laparoscopic surgery before. Thus, we scheduled her for a repeat operation for further treatment of her hernia.

Although she had a laparoscopic hernia repair previously, it was obvious that the mesh wasn’t placed low enough to cover the entire hernia defect, or the hole in the muscle. At her surgery, the small intestine was stuck in the hernia defect and had to be pulled out prior to repairing the hole. A ‘tension free’ repair was performed.
Click here to close
7. Recurrent incisional hernia after colon surgery in a 42 year old male.
This 53year old male patient had colon surgery for cancer 3 years ago. After his surgery, he developed a bulge at the incision. He was diagnosed with an incisional hernia and underwent laparoscopic incisional hernia repair by a surgeon in his area. This surgery went well initially, but after about 6 months, he noticed that the bulge had returned.
He saw his initial surgeon again who ordered a CAT scan of the abdomen.
His surgeon told him that there was no recurrent hernia, and that his abdominal muscles were weak, causing the bulging under the skin. He was told that there was almost nothing that could be done.
The patient sought a second opinion at California Hernia Specialists where we reviewed his CAT scan and examined his abdomen. It was clear that although his muscles had weakened, there was also a definite hole in the muscle and a recurrent incisional hernia. His small bowel and internal fat was protruding through the hole contributing to his bulge.
The 3 CAT scan images below show the patients normal muscles above the hernia, then a large hernia defect or hole in the muscle, and then the normal muscles again below the hernia defect.


Because this patient had failed two prior surgeries, we performed a complex open hernia repair on him. This repair included a technique called ‘component separation’, where the oblique muscles on the sides of the abdomen, are partially released, or cut, to allow the rectus muscles to be pulled back together in the middle of the abdomen.
Since the abdominal muscles were weakened, we placed a sheet of biologic mesh under the muscle in the middle at the area of the hernia hole, closed the muscle over this mesh, then placed another mesh on top of the muscles which were closed. This provided him with three layers of repair.
The CAT scan image below compares the patient before surgery, and then after surgery when the muscle has been pulled back together and the hernia has been repaired.

The patient is doing great months after his surgery with no bulge, no pains, and the ability to return to normal activities. He’s lost close to 40 pounds since he can now exercise again and is feeling back to normal.
Click here to close
8. Open Sports Hernia Repair on a 54 year old athlete.
This patient had almost 6 years of left groin pain. He was an avid athlete and had felt a ‘tear’ in his left groin. Ultrasounds and CT scans failed to show an inguinal hernia however his pain continued. Over the years, the pain got worse and traveled further up and down his groin.
Ultimately he sought help at California Hernia Specialists where a tentative diagnosis of a sports hernia was made based on his symptoms. No inguinal hernia could be felt on examination before surgery.
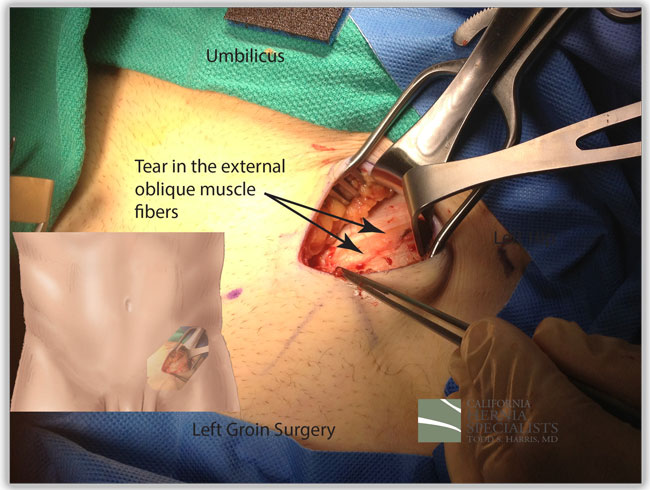
The intra-operative photo above shows an obvious tear in the external oblique, which is the outer layer of muscle in the groin. In the photo, the yellow fat from underneath the muscle is seen between two edges of the white muscle fascia which have torn. The tear was about 4 inches long, and about a 0.5 inch wide. This was repaired with a mesh under the tear, and by closing the tear with sutures.
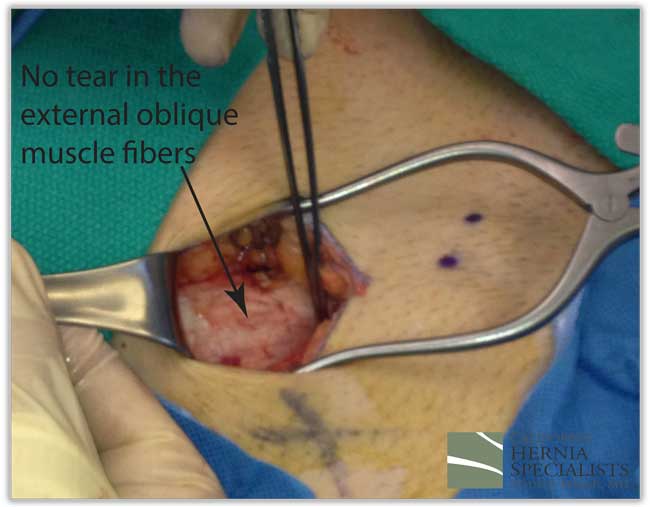
The photo below shows a normal external oblique which is white throughout with no yellow of fat from underneath and no tear.
On recent follow-up, the patient is having no more pain in his left groin and is back to elite athletic activities on a full time basis.
Click here to close
9. A very rare Spigelian hernia in an otherwise healthy 35 year old.
This patient had been referred to several medical doctors due to a swelling of the right side of the abdomen. Initially his doctors assumed that he had a pulled muscle or a muscle strain. However, over the following months, the right side of his abdomen continued to get larger. Ultimately his medical doctor ordered a CAT scan which is shown below.
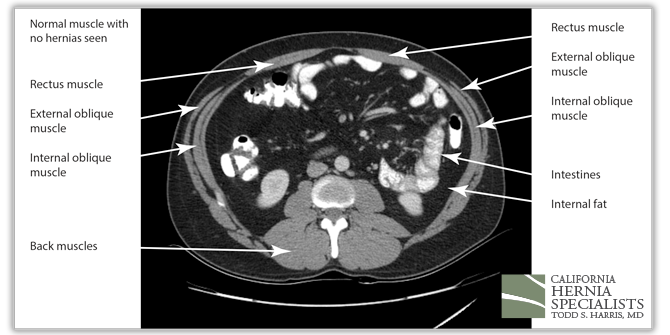
The above image shows the upper part of this patients abdomen. No hernia is seen here; only normal muscles.

This image above is slightly lower on the abdomen. Only the fat from the hernia is seen. The actual hole in the muscle, or the hernia defect, is not seen yet.

The above CAT scan image shows the hole in the muscle with the fat pushing through the defect.
This image shows the normal muscles in the lowest part of the abdomen
Laparoscopic hernia surgery was performed for this patient. The internal fat which was pushing through the hernia defect was pulled back into the abdomen. The hole in the muscle was identified and a large lightweight mesh was placed under the muscle and secured in place. The patient recovered very well from the surgery and is back to normal activity without the large bulge in his right abdomen.
The simulated CAT scan picture of what this would look like is shown below along with a comparison between the before and after images.

 Click here to close
Click here to close
10. A young women with a recurrent hernia immediately after another surgeons repair.
This women had presented to another surgeon with the complaint of a bulge in her left groin. The surgeon performed an open hernia repair and in his operative report said that she had a “direct inguinal hernia” and “absolutely no femoral hernia was seen”. However, immediately after surgery she noticed a clear bulge in the exact same spot as she saw before his surgery.
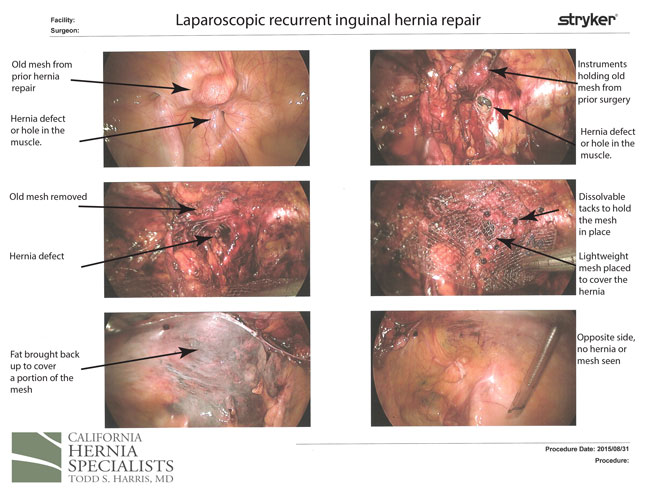
Thus, she presented to California Hernia Specialists for a second opinion. We ordered an ultrasound which showed a hernia still located in the left groin. Due to the fact that she had just undergone an open surgery, we offered her a laparoscopic hernia repair in the left groin. We were not sure what we would see at the time of surgery since the prior surgeon said he clearly did not find a femoral hernia.
At the time of our surgery, we saw the prior surgeons use of an older ‘plug’ type hernia mesh located in the ‘direct hernia’ space. However, we saw a very clear femoral hernia just below this direct hernia. To adequately repair the femoral hernia, we had to remove the prior plug, and cover the entire area with a laparoscopic mesh.
The patient did great and has not had a recurrent bulge since her surgery. The images below are from her surgery
 Click here to close
Click here to close
11. Large, long-standing, groin hernias which extended into the scrotum.
Patients often ask me if or when they should have their hernia repaired. There is no simple answer except there are a few basic rules of thumb as to when to have surgery for your hernia:
- if the hernia begins to limit your activities
- if the hernia is getting larger over time
- if you are having difficulty reducing the hernia back into your abdomen
Patient 1
6 months post surgery

Patient 2:
3 months post surgery

Patient 3:
Patient 4:

Patient 5:

Patient 6:

Patient 7:

Patient 8:

Click here to close





















